What is Sciatica Endometriosis
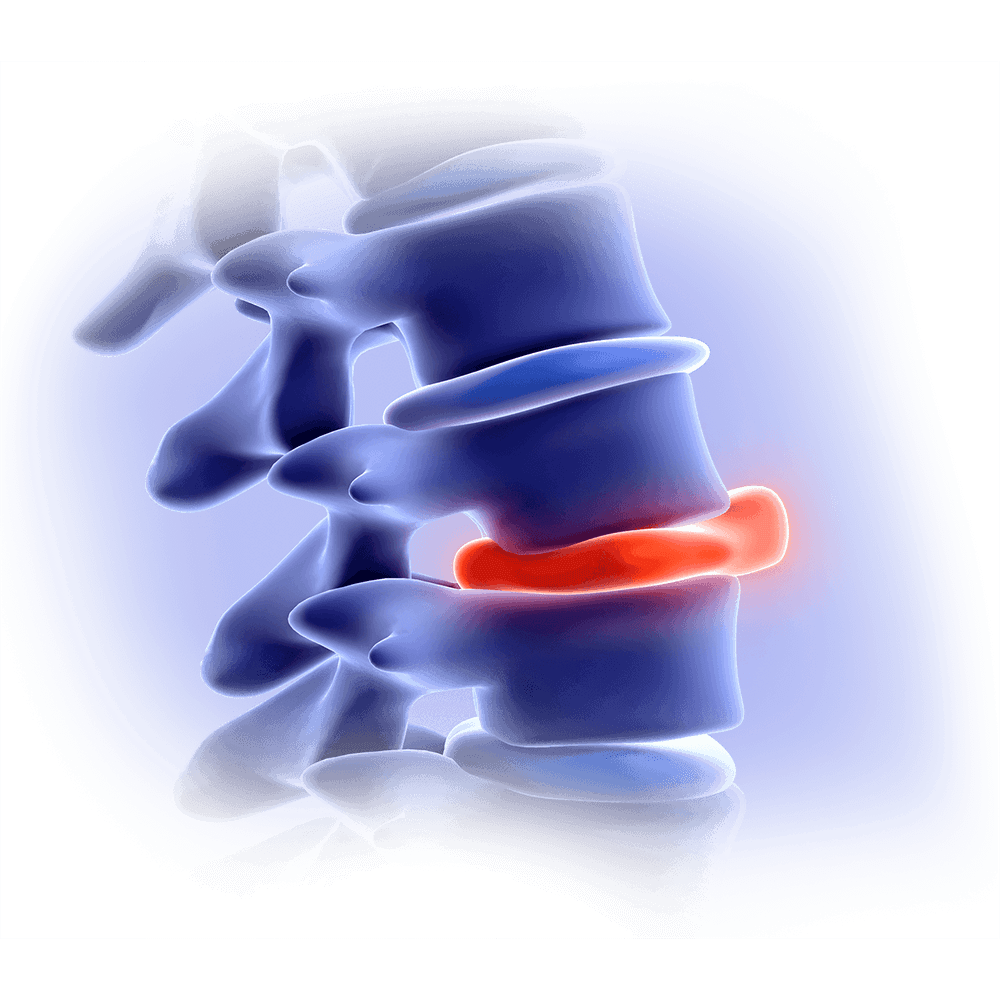
Endometriosis occurs when tissue similar to the uterine lining grows outside the uterus. While it usually affects the ovaries, fallopian tubes, or pelvic lining, in rare cases these lesions can attach to the sciatic nerve — one of the largest and most important nerves in the body. This nerve runs from the lower spine, through the pelvis, and down each leg.
When endometrial lesions grow close to the nerve, they can compress or infiltrate it, causing inflammation and severe pain. What makes this form of endometriosis particularly challenging is its cyclical nature: symptoms often worsen before or during menstruation, reflecting the hormonal changes that drive the disease.

The connection between Sciatica and Endometriosis
Although sciatica and endometriosis are generally treated as separate conditions, there are cases where the two are closely connected. When endometrial tissue grows near the lumbar nerve roots or directly on the sciatic nerve, it can provoke intense, debilitating pain that mimics classic sciatica. Patients often experience radiating pain, numbness, or weakness in the leg, and conventional therapies may not provide lasting relief.
Because of the unusual origin of the pain, precise, minimally invasive surgical access is often essential. Such procedures allow surgeons to reach the affected areas safely and address nerve irritation effectively, which can be particularly challenging when endometriosis is involved.
Why Sciatic Pain Can Be a Sign of Endometriosis
The pain caused by sciatic endometriosis often begins subtly — a dull ache in the hip, buttock, or leg that seems to come and go with the menstrual cycle. Over time, it can develop into a sharp, burning, or shooting pain that radiates from the pelvis down one leg, sometimes reaching as far as the foot. Many women describe a sensation of heaviness, numbness, or tingling that worsens before or during menstruation. These symptoms are frequently mistaken for a spinal disc problem, which explains why sciatic endometriosis can remain undiagnosed for years.
The reason this happens lies in the way endometriosis behaves inside the body. Normally, the tissue that lines the uterus thickens and sheds with each menstrual cycle. In endometriosis, similar tissue grows outside the uterus — and in rare cases, it attaches to or around the sciatic nerve. Each month, these misplaced cells respond to hormonal changes by swelling and bleeding internally, causing inflammation and scarring. Over time, this process irritates or compresses the nerve, producing pain that feels identical to typical sciatica.
In addition, hormonal fluctuations can worsen inflammation, while previous pelvic surgery or untreated deep endometriosis may allow the disease to spread toward the nerve pathways. The result is a cycle of irritation, nerve damage, and pain that mirrors traditional sciatica but has a very different origin. Recognizing this connection is essential, because treating only the spine or lower back will not resolve the true cause.
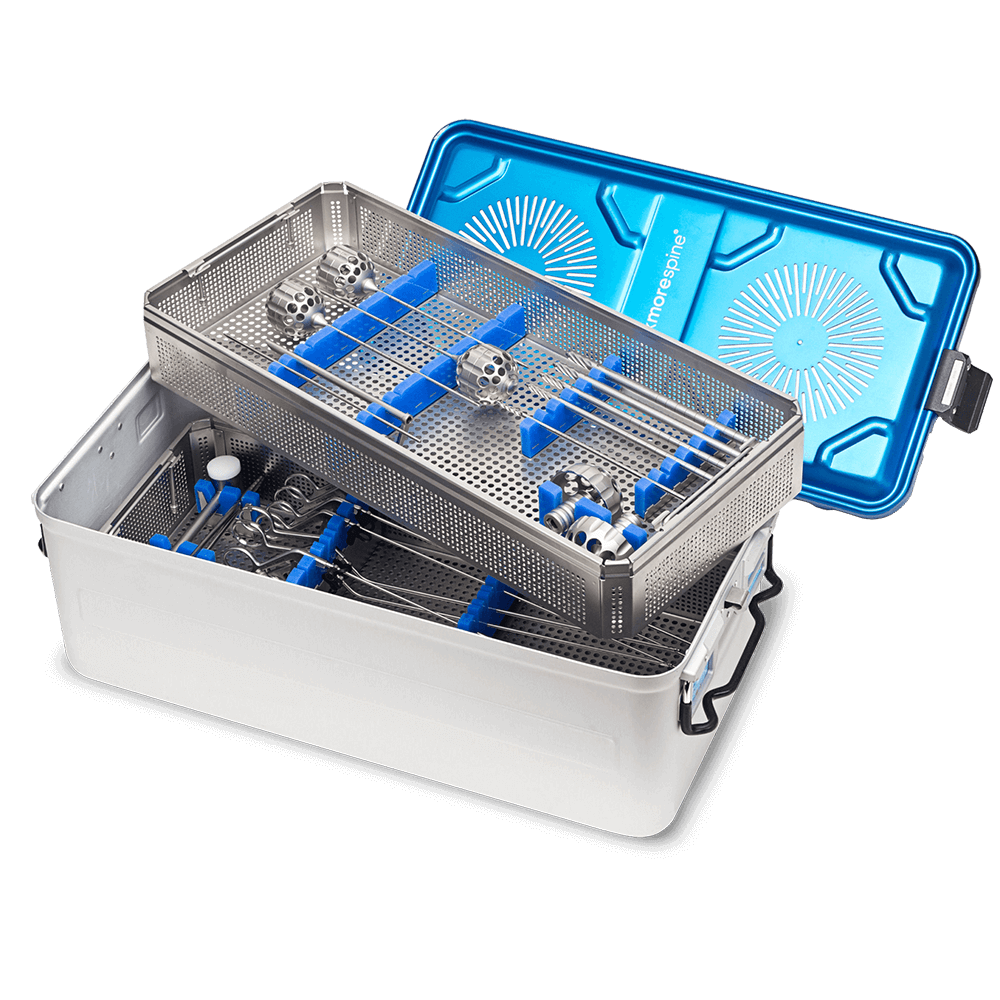
Designed for minimally invasive surgery
Endoscopic surgery is a modern, minimally invasive procedure that offers significant advantages over traditional spine surgery. Such as:
-
Shorter hospital stays, often same-day discharge
- Minimal tissue damage due to targeted access
- Effective relief from nerve pain
-
Faster return to daily activities
-
Reduced risk of complications and spinal instability
Minimally Invasive Solutions for Complex Cases
The most effective treatment for sciatic endometriosis is surgical removal of the endometriotic tissue, ideally performed by a specialist familiar with pelvic nerve surgery. During laparoscopic nerve decompression, the surgeon carefully excises the lesions while preserving healthy nerve structures. In some cases, hormonal therapy is used afterward to reduce the risk of recurrence and to suppress any remaining microscopic disease.
Recovery varies depending on how deeply the nerve was affected. Many patients notice an immediate reduction in leg pain, followed by gradual improvement in strength and mobility. Physical therapy can also help the nerve heal and restore full function. The key is early, precise intervention — once nerve damage becomes chronic, recovery is far more difficult.
Transforaminal Endoscopic Spine Surgery
MaxMoreSpine Expertise
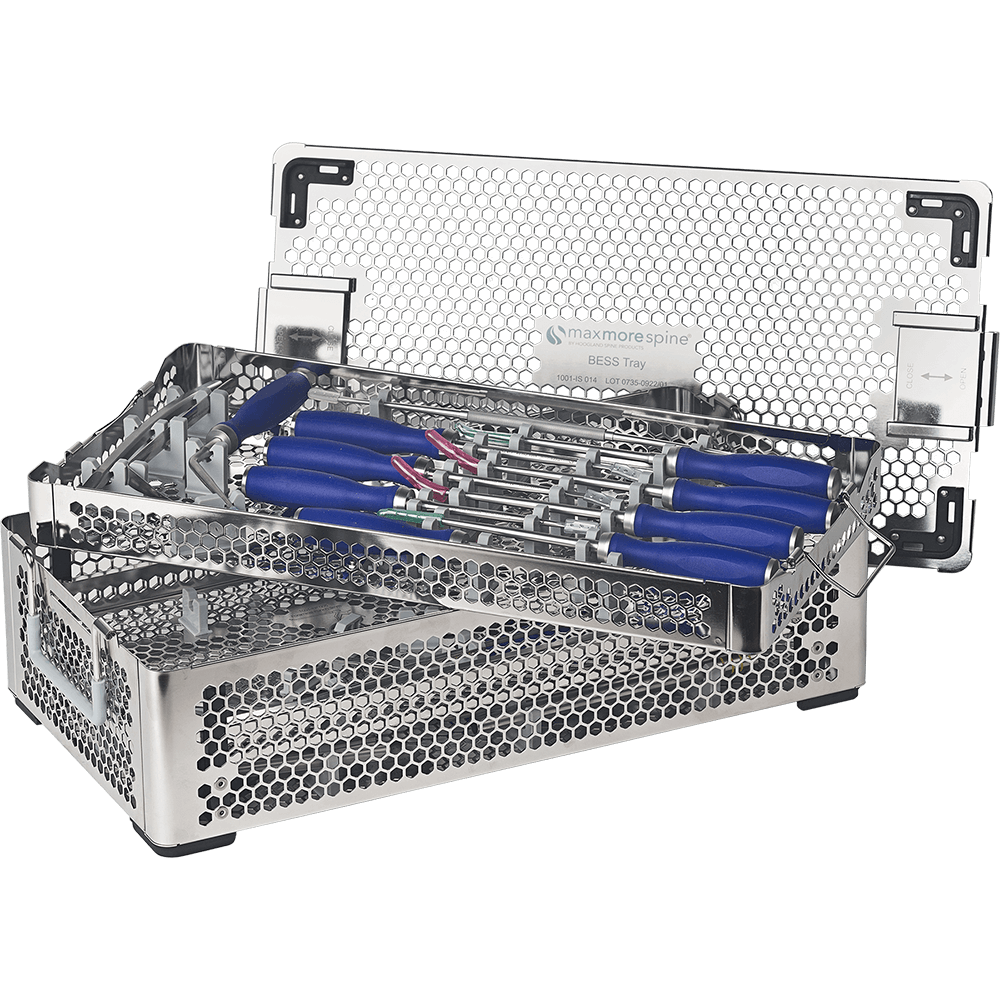
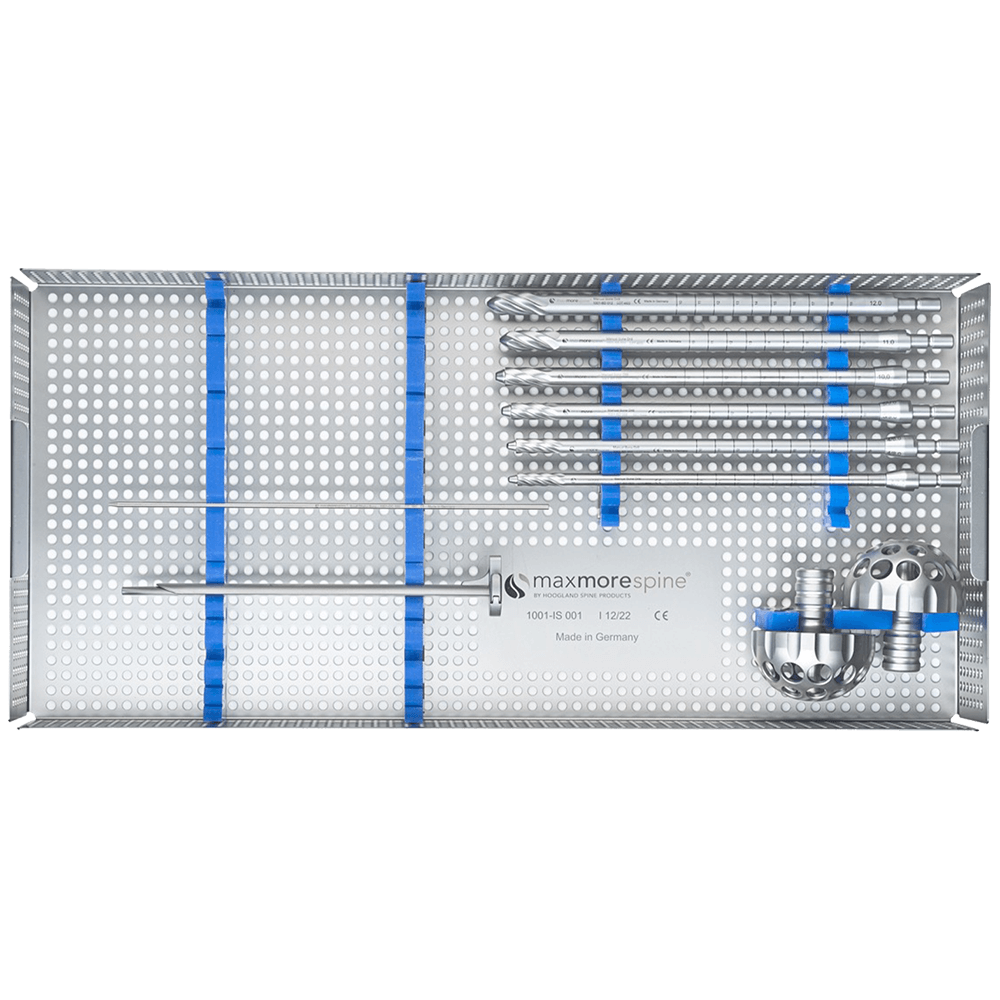
Endoscopic spine surgery offers a modern, minimally invasive approach that provides significant advantages compared to traditional spine surgery. By allowing targeted access to affected nerves with minimal tissue disruption, this technique reduces recovery time, alleviates nerve pain, and lowers the risk of complications or spinal instability. Patients often experience faster relief and a quicker return to daily activities, making it a highly effective option for conditions where sciatica and endometriosis intersect.
At MaxMoreSpine, our endoscopic instruments are specifically designed to help surgeons navigate these challenging cases with the highest degree of precision and safety. Our technology supports accurate treatment of nerve-related pain while minimizing tissue damage, enabling better outcomes for patients with complex lumbar conditions.

PTED Endoscopic System
Neurological safety during transforaminal endoscopic surgery of the spine is of paramount importance.
PSLD Endoscopic System
Lumbar spinal decompression is performed with a posterior interlaminar approach.
MAXDISC® Endoscopic System
MaxDisc ® provides treatment for patients who have failed conservative care and are not yet ready for major surgery.
MINI Endoscopic System
Although conventional procedures show fine results, continuous technical optimization should be the goal.
Joint Ablation System
The J@blation system is exclusively designed as a system to treat facet joints.
Biportal Endoscopic System
omes out to be one of new trends of treatment of degenerative spine disorders.
MaxFusion by Dr. Morgenstern
Endoscopic / Percutaneous Transforaminal Lumbar Interbody Fusion System.